••••
ALDINE ISD
Library

Welcome Aldine ISD Employees!
Here, you will be able to access and view your 2024 benefits plan options. These videos and resources are designed to provide you the information you need to maximize your benefits.
This video provides a high-level overview of your benefits offering for next year. Click the 2024 Benefits link for complete details and the Enroll now button to enroll today.
Medical and Rx
Mental Health Resources and EAP
Dental and Vision
Disability
Employee Perks
Life and Voluntary Life
Additional Voluntary Benefits

Benefits Video Library

Benefit Terms Explained
FSAs

Voluntary Benefits Overview

403(b) Retirement Plans

529 College Savings

Employee Assistance Programs
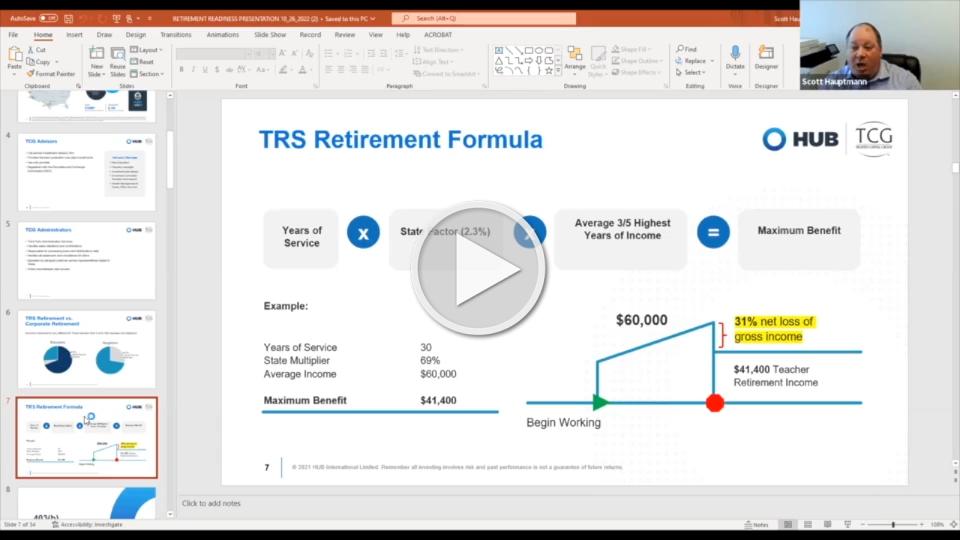
Retirement Readiness Presentation

HSA Presentation
Open Enrollment Presentation

Kelsey-Seybold Open Enrollment Presentation
Introduction to Medicare
Contact a Benefits Outlook representative at 855.474.9494